AbstractA 25-year-old Uzbek male presented with right upper abdominal pain for 20 days. On radiologic studies, a huge cystic mass was noticed in the right liver which was suspected as parasitic. The patient received right hepatic segmentectomy (segment 7), and the surgically resected mass was confirmed as cystic echinococcosis (CE), measuring 10.5 cm in its diameter. The inner surface of the cyst was bile-stained. The patient was discharged on the 8th hospital day, and was rechecked 6 months after the surgical intervention without any evidence of recurrence. The present report describes findings of an imported case of CE which represented ultrasound images of the 'ball of wool'.
INTRODUCTIONEchinococcosis or hydatid disease (HD) is a parasitic disease infected by a cystic larval form of the cyclophyllidean tapeworm, Echinococcus. Human is one of its intermediate hosts, which include sheep, cattle, goats, rodents, marsupials, and other herbivorous mammals. Four taxonomically relevant species of the genus Echinococcus are infecting humans; E. granulosus, E. multilocularis, E. vogeli, and E. oligarthrus. Among them, E. granulosus and E. multilocularis mainly cause zoonotic infections of public health importance, cystic echinococcosis (CE) and alveolar echinococcosis (AE), respectively. The remaining 2 species may infect humans but are rarely found in limited areas of South America [1].
Both CE and AE are distributed globally as endemic diseases of pastoral environment and commonly found among sheep- or cattle-raising people [2]. CE commonly involves the liver and lungs but AE involves almost the liver in humans. However, cases of HD occur worldwide nowadays and regarded as a global emerging disease. Moreover, patients with unusual, atypical, or complex type of HD have been reported increasingly [3,4]. Furthermore, HD is often confused with malignancy or other diseases in non-endemic areas. Since HD develops silently, it used to be neglected in public health points of view, and most of the cases face difficulty for rapid and correct diagnosis in non-endemic areas [4].
CASE DESCRIPTIONA 25-year-old Uzbek male was referred to the Department of Surgery, Dongsan Medical Center, Daegu, Korea on 8 January 2012, due to a cystic mass in the liver which was found by computed tomography at a private clinic. He had complained of right upper abdominal pain for 20 days. He has been in Korea for 3 years as a worker. Dull abdominal pain had progressed in its intensity day by day. He had no history of past illness and denied any contact history with domestic animals or pets as well as livestock in Uzbekistan. On physical examination, icterus was absent, and mild tenderness was recognized in the right upper abdomen without any palpable mass. He showed normal ranges of hemoglobin, white blood cell counts, including eosinophils, electrolyte profiles, and chemistry, including liver enzymes and bilirubin. His tumor markers, alpha-fetoprotein, carcinoembryonic antigen, and carbohydrate antigen 19-9, were within normal limit. CT from a private clinic recognized a 10×9 cm-sized hypoattenuating mass with focal wall calcifications at the liver segment 7 (Fig. 1). Ultrasound examinations observed an oval and well-encapsulated echogenic mass with internally compactly filled tubular structures in the subcapsular location of the right posterior liver. MR image showed an oval mass with heterogeneous contents and without further contrast enhancement of this mass after intravenous administration of MR contrast (Primovist®; Bayer HealthCare, Seoul, Korea). Serologic test by ELISA to detect specific antibodies to parasite antigens, including Echinococcus, Clonorchis sinensis, Paragonimus westermani, cysticercus, and sparganum (absorbance at 450 nm) was in negative ranges. Regardless of this uncertain clinical setting, the liver mass was strongly suspected as parasitic because ultrasonography showed a round cyst with tubular folding contents. Those images suggested a cyst of foreign body materials. Moreover, because the patient had a large atypical cystic mass, and abdominal pain appeared suddenly and progressed continuously, surgical resection of the mass was decided.
He underwent hepatic segmentectomy (Segment 7). On intraoperative ultrasound, these tubular contents were more clearly visualized (Fig. 1). Grossly, the right hepatic mass showed a relatively well-demarcated, round, pale tan to red, smooth and cystic appearance, measuring 10.5×8.7×4.2 cm and 163.5 g. The cut-surface of the right hepatic mass showed a large unilocular cyst, containing olive-colored soft and flabby membrane attached with several small spherical brown clayish and soft nodules (Fig. 2). Microscopically, the hepatic mass consisted of outer thick adventitial layer, thick laminated gelatin layer in the middle, and inner thin germinal layer with numerous scattered protoscolices of E. granulosus in bile-tinged fluid and necrotic debris. The protoscolices had suckers and calcium corpuscles (Fig. 2). Some of them looked degenerated, and some of them were found intact in their morphology. Although thick bile like content was filled in the cystic mass, biliary communication was not noticed.
After the surgery, the patient recovered his health well and was discharged on the 8th hospital day without any complication. No anthelmintic drug was medicated postoperatively because the cystic mass was completely resected. The patient had been working well without evidence of recurrence for 6 months after the operation.
DISCUSSIONCorrect clinical diagnosis of CE is important for proper management of hepatic echinococcosis. The clinical diagnosis should include differential diagnosis of CE and its staging before any intervention because CE is a chronic years-long disease which is treated by several options according to its stage [7]. The stage of CE was classified by WHO experts in 2003 [8] and reproposed in relation with diagnosis and treatment in 2010 [7]. For management of clinically diagnosed CE, one option among surgical removal, drainage and chemotherapy, chemotherapy alone, and watch and wait is recommended according to its stage and size [4,7].
The cystic mass of the present case was diagnosed as CE based on images and histopathologic findings. His CT findings recognized a spherical cyst with calcification in the right liver segment 7. The ultrasound images visualized little fluid in the cyst but folding materials showed an image of so-called "ball of wool" (Fig. 1). The image was compatible with that of the stage CE4 [7,8]. The CE4 stage is regarded as inactive. The gross findings of the surface or cut-edge of the present cyst were also looking inactive (Fig. 2). The present cyst was filled not by clear cystic fluid but by folding septum and gelatin tissue mixed with thick bile-stained mucus. This cyst finding is compatible with a process of natural degeneration of inactive CE, and the same degenerating process has been described after chemotherapy [3].
The histopathological finding of the present liver cyst demonstrated typical microscopic morphology of CE (Fig. 2). The ball of wool in the mass by ultrasound scanning was images of septations and folds in the cyst. However, the cyst wall was well-outlined, and some protoscolices were found intact while many of them were degenerating (Fig. 2). These morphologic findings were compatible with the stage CE4 as a whole, but there was a possibility of some remaining live protoscolices in the present CE. Thousands of protoscolices are produced in 1 CE during the active stage but they may lose their viability one by one after the transition stage. The process may take a years-long period. Although it is difficult to confirm their viability by morphologic findings, some of them might have been viable.
Clinical diagnosis of CE is commonly supported by both images and serology [7]. Serology of the present case was negative for specific IgG antibodies to a fluid antigen of E. granulosus by ELISA. The negative serology made clinical diagnosis of the present case difficult before the surgical intervention. The sensitivity of ELISA using cystic fluid is known as 85-98% for liver cysts, 50-60% for lung cysts, and 90-100% for multiple organ cysts [7]. Clinically, the sensitivity is inversely related to the degree of sequestration of the echinococcal antigens in the cyst. Ruptured cysts are associated with strong immune responses, whereas intact or healthy cyst can elicit a minimally detectable response [7]. Specific antibody levels of this patient against cyst fluid antigen by ELISA revealed negative reaction. The ELISA using fluid antigen demonstrated false negative reaction up to 15% possibly due to immune status of the infected individuals, especially in case of inactive CE.
The present patient complained of progressive abdominal pain which was induced by the CE mass. The present cyst was compatible with the stage CE4, which is inactive and managed by watch and wait [4,7]. However, the present case had localized pain which was relieved by surgical resection of the CE. The pain must have originated by a complicated CE due to the big size of the cyst, 10.5 cm in diameter [9]. In the present case, surgical removal was inevitable to relieve pain and accomplish a definitive treatment.
The present patient was an Uzbek and had stayed in Korea for 3 years. The cyst size was big which suggested he was infected several years before. Since Uzbekistan is an endemic area of CE [10], this patient should be an imported case of CE in Korea. Already 6 cases have been reported to have been imported from Uzbekistan in Korea [5].
The present report describes clinical findings of an imported case of CE which represented ultrasound images of an inactive stage of CE4. However, a few intact protoscolices may have remained in the cyst, and pain may have occurred due to the big size of the mass.
REFERENCES1. D'Alessandro A, Rausch RL. New aspects of neotropical polycystic (Echinococcus vogeli) and unicystic (Echinococcus oligarthrus) echinococcosis. Clin Microbiol Rev 2008;21:380-401. PMID: 18400802.
2. Grosso G, Gruttadauria S, Biondi A, Marventano S, Mistretta A. Worldwide epidemiology of liver hydatidosis including the Mediterranean area. World J Gastroenterol 2012;18:1425-1437. PMID: 22509074.
3. da Silva AM. Human echinococcosis: A neglected disease. Gastroenterol Res Pract 2010;pii: 583297 Epub 2010 Aug 31.
4. Brunetti E, Garcia HH, Junghanss T. International CE Workshop in Lima, Peru, 2009. Cystic echinococcosis: Chronic, complex, and still neglected. PLoS Negl Trop Dis 2011;5:e1146. PMID: 21814584.
5. Byun SJ, Moon KC, Suh KS, Han JK, Chai JY. An imported case of echinococcosis of the liver in a Korean who traveled to western and central Europe. Korean J Parasitol 2010;48:161-165. PMID: 20585534.
6. Kim SJ, Kim JH, Han SY, Kim YH, Cho JH, Chai JY, Jeong JS. Recurrent hepatic alveolar echinococcosis: Report of the first case in Korea with unproven infection route. Korean J Parasitol 2011;49:413-418. PMID: 22355210.
7. Brunetti E, Kern P, Vuitton DA. Writing Panel for WHO-IWGE. Expert consensus for the diagnosis and treatment of cystic and alveolar echinococcosis in humans. Acta Trop 2010;114:1-16. PMID: 19931502.
8. WHO Informal Working Group. International classification of ultrasound images in cystic echinococcosis for application in clinical and field epidemiological settings. Acta Trop 2003;85:253-261. PMID: 12606104.
9. Nunnari G, Pinzone MR, Gruttadauria S, Celesia BM, Madeddu G, Malaguarnera G, Pavone P, Cappellani A, Cacopardo B. Hepatic echinococcosis: Clinical and therapeutic aspects. World J Gastroenterol 2012;18:1448-1458. PMID: 22509076.
10. Torgerson PR, Oguljahan B, Muminov AE, Karaeva RR, Kuttubaev OT, Aminjanov M, Shaikenov B. Present situation of cystic echinococcosis in Central Asia. Parasitol Int 2006;55:S207-S212. PMID: 16361112.
Fig. 1Radiologic findings. (A) Preoperative axial contrast-enhanced abdominal CT scan shows an oval, hypoattenuating mass, like cystic mass, with small wall calcifications (arrow). (B) Intraoperative ultrasound shows clear delineation of tubular structures, so-called "ball of wool" appearance. 
Fig. 2Gross appearance (A, B) and histopathologic findings (C, D) of the surgically removed liver cyst. (A) Grossly, the right hepatic mass shows a relatively well-demarcated, round, pale tan to red, and smooth and cystic appearance, measuring 10.5×8.7×4.2 cm and 163.5 g. (B) The cut surface of the resected specimen shows unilocular cyst, containing olive-colored soft flabby transparent membrane, attached with several small spherical brown clayish soft nodules. (C) Membranous fragments of laminated (arrowhead) and germinal layers (thin arrow) are seen with a few protoscolices of E. granulosus (H&E, ×100). (D) Laminated cyst walls and germinal layers are seen with intact protoscolices of E. granulosus (arrowhead) (H&E, ×400). 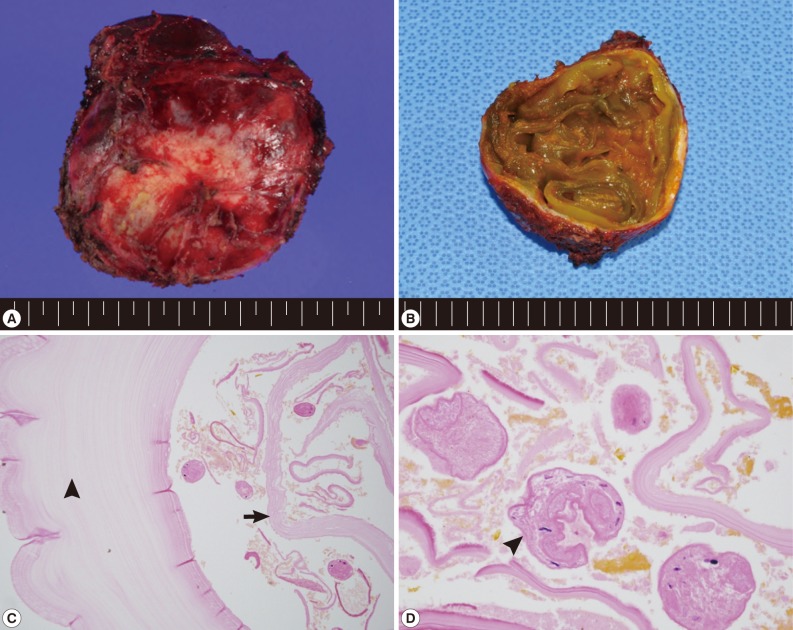
|
|
|||||||||||||||||||||||||||||||||||||||||||