AbstractIn this study, we found that Haplorchis taichui, a heterophyid intestinal fluke, is highly prevalent, with heavy worm loads, among riparian people in Saravane and Champasak province, Lao PDR. Fecal specimens were collected from 1,460 people (717 men and 743 women) in 12 riparian (Mekong river) districts and were examined by the Kato-Katz fecal smear technique. The overall helminth egg positive rate was 78.8% and 66.4% in Saravane and Champasak province, respectively. The positive rate for small trematode eggs (STE), which included H. taichui and other heterophyids, Opisthorchis viverrini, and lecithodendriids, was 69.9% and 46.3% in Saravane and Champasak province, respectively. To obtain adult flukes, 30 STE-positive people were treated with 40 mg/kg praziquantel and then purged. Whole diarrheic stools were collected 4-5 times for each person and searched for fluke specimens using a stereomicroscope. Mixed infections with various species of trematodes (H. taichui, Haplorchis pumilio, O. viverrini, Prosthodendrium molenkampi, Centrocestus formosanus, and Echinochasmus japonicus) and a species of cestode (Taenia saginata) were found. However, the worm load was exceptionally high for H. taichui compared with other trematode species, with an average of 21,565 and 12,079 specimens per infected person in Saravane and Champasak province, respectively, followed by H. pumilio (41.9 and 22.5, respectively) and O. viverrini (9.4 and 1.5, respectively). These results show that diverse species of intestinal and liver flukes are prevalent among riparian people in Saravane and Champasak province, Lao PDR, with H. taichui being the exceptionally dominant species.
INTRODUCTIONFoodborne liver and intestinal flukes are important groups of parasites from the public health point of view [1-4]. Lao Peoples Democratic Republic (Lao PDR) is located in the middle of the Indochina Peninsula, and the Mekong River runs through the whole length of the country from north to south. Until the 1990s, the liver fluke Opisthorchis viverrini and soil-transmitted nematodes, including Ascaris, Trichuris, and hookworms, were the major helminths prevalent among the Laotian people [5-8].
In 1991, Haplorchis taichui adult flukes were recovered for the first time from 5 Laotian students studying in Czechoslovakia [9]. Since then, other intestinal flukes, including Haplorchis pumilio, Haplorchis yokogawai, Prosthodendrium molenkampi, Phaneropsolus bonnei, Centrocestus formosanus, Echinostoma revolutum, Artyfechinostomum malayanum, Echinochasmus japonicus, and Euparyphium sp. have been recovered from infected residents of Vientiane municipality, Phongsaly, Saravane, Khammouane, and Savannakhet province [10-16]. The predominating species and the the intensity of infection with each fluke species varied by locality. For example, O. viverrini infection was predominant over H. taichui in Vientiane municipality, whereas H. taichui infection was dominant over O. viverrini in Saravane province [10]. On the other hand, in Phongsaly Province, located in the northernmost area of Lao PDR, high prevalences of H. taichui and H. yokogawai were detected with no detection of O. viverrini [15].
After completion of the international collaboration project [10,11,14] between the Korea Association of Health Promotion and Ministry of Public Health (MOPH), Lao PDR on the control of intestinal helminthiases in Lao PDR from 2000-2004, a new 5-year project plan was started in 2007 to control foodborne trematode infections by the Korea Foundation for International Healthcare and MOPH, Lao PDR [15,16]. In this new project, the primary goal was to control opisthorchiasis in endemic areas and to reduce the incidence of cholangiocarcinoma in the Mekong River basin.
For the successful implementation of this project, a desirable pre-requisite should be the elucidation of the actual status of infection with O. viverrini in each target village. The recovery of eggs only in the feces is not sufficient for this purpose, because the eggs of O. viverrini and those of minute intestinal flukes are practically indistinguishable in routine fecal examinations. The present study was performed to determine the actual status of infection with foodborne trematodes by recovery of adult flukes from riparian people of Saravane and Champasak province, Lao PDR.
MATERIALS AND METHODSSaravane province (capital city, Saravane) is located about 500 km south from Vientiane, and Champasak province (capital city, Pakse) is located nearby and just south of Saravane province (Fig. 1). Small riverside villages, each having 200-300 residents, located near the mainstream or tributaries of the Mekong River were selected for this study, which included 12 villages (in 6 districts) in both Saravane and Champasak province. Most villagers were agricultural workers, and some had caught freshwater fish from small streams and ponds and consumed them raw or improperly cooked.
A total of 1,460 fecal samples (1 sample per person) were collected from the villagers (717 men and 743 women, 12-82 years-of-age) from December 2009 to June 2010. Samples were transported to the Malaria Stations in Saravane and Champasak province within 2-3 days of collection and were stored at 4℃ until examined. The Kato-Katz thick smear technique was used to detect helminth eggs. Trematode eggs 23-32 µm in size were collectively recorded as small trematode eggs (STE). Fecal examinations and anthelmintic treatments were officially approved by the Ministry of Public Health, Laos, under the terms of the Korea-Laos Agreement on Foodborne Trematodiases Control in Laos (2007-2011).
Thirty people who were positive for STE were selected for adult worm recovery at the Malaria Station. After obtaining informed consent, they were treated with a single oral dose of 40 mg/kg praziquantel (Distocide@; Shinpoong Pharm., Seoul, Korea) and then purged with 30 g magnesium salt. Whole diarrheic stools passed successively 4-5 times were collected and pooled individually. Diarrheic stools were processed as previously described [10,11]. Worms were collected using a glass pipette and were washed several times in water. Worms were counted and some were fixed with 10% formalin under cover slip pressure, acetocarmine-stained, and morphologically identified using a light microscope.
Fecal examination results were analyzed using the Student's t-test and the chi-square test. P-values<0.05 were considered statistically significant.
RESULTSFecal examinationThe overall helminth egg positive rate was 78.8% and 66.4% in Saravane and Champasak province, respectively (Table 1). There were some mixed infection cases involving different kinds of nematodes, trematodes, and cestodes. The most highly prevalent was STE, which included eggs of O. viverrini, heterophyids, and lecithodendriids, with a prevalence of 69.9% (46.5-87.2% by district) and 46.3% (7.5-73.9% by district) in Saravane and Champasak province, respectively (Table 1). The district showing the highest STE prevalence was Toumlane (87.2%) in Saravane province and Pathumphon (73.9%) in Champasak province. Paksong, an urban area of Champasak province, displayed the lowest STE prevalence (7.5%) among the 12 districts surveyed. Other parasite eggs detected in Saravane and Champasak province included hookworms (20.1% and 22.1%, respectively), Ascaris lumbricoides (5.7% and 4.0%, respectively), Trichuris trichiura (0.8% and 5.6%, respectively), Taenia spp. (2.3% and 4.3%, respectively), and Trichostrongylus sp. (7.6% and 2.5%, respectively). The egg positive rates were not significantly (P>0.01) different between men and women (data not shown).
Worm collectionThe adult worm collection was completed in 30 people (15 men and 15 women; 20-65 years; 19 in Saravane and 11 in Champasak) (Table 2). A total of 543,852 helminth specimens were recovered (average of 18,128 per person; range 6-129,238 worms per person). Intestinal flukes were recovered in all 30 cases (100.0%), and O. viverrini was recovered in 17 cases (56.7%). The total number of H. taichui specimens recovered in Saravane and Champasak province were 409,738 (n=19; average 21,562 per person) and 132,865 (n=11; average 12,078 per person), respectively, which was markedly higher than the other helminth parasite species (Table 2). The next most frequent species was H. pumilio, with 796 (n=19; average 41.9 per person) and 247 (n=11; average 22.5 per person) in Saravane and Champasak province, respectively (Table 2), followed by O. viverrini, with 179 (n=19; average 9.4 per person) and 17 (n=11; average 1.5 per person) in Saravane and Champasak province, respectively (Table 2). Small numbers of specimens were collected for Taenia saginata, C. formosanus, P. molenkampi, and E. japonicus from a small number of people (Table 2). Two Haplorchis spp. comprised 99.96% (99.95% and 99.98% in Saravane and Champasak province, respectively) of the total helminth specimens recovered, whereas O. viverrini comprised only 0.04% (0.04% and 0.01% in Saravane and Champasak province, respectively). The highest worm load of H. taichui collected from a single person was 129,159 in Champasak province, followed by 97,791 and 71,647 in Saravane province.
DISCUSSIONAn extremely high predominance of intestinal flukes, in particular, H. taichui, was evident in Saravane and Champasak province. The liver fluke, O. viverrini, constituted only a very small portion of the helminths infected among the riparian people in the surveyed localities. Therefore, we could confirm that the real O. viverrini heavy endemic areas in Lao PDR include Vientiane municipality and Savannakhet province, based on the previous results from our research group [10,11]. Haplorchis spp. dominate in Khammouane, Saravane, and Champasak provinces with only a low-grade endemicity of opisthorchiasis, based on our previous observations [10,14] and those of the present study. Phongsaly province [15] and Luang Prabang and Xiengkhouang provinces are also Haplorchis-dominant areas without O. viverrini endemicity (to be published).
The individual worm load of H. taichui was extremely high in this study, particularly in Saravane province. It was 67 times higher than in Khammouane province (324 vs. 21,565) [14], 209 times that of Savannakhet province (103 vs. 21,565) [11], and 799 times that of Vientiane municipality (27 vs. 21,565) [10]. Indeed, it was even 3-times higher than that of our previous study in Saravane province [10]. This may have been due to the fact that different districts were surveyed in our earlier and present studies. The present report of intestinal flukes, including H. taichui and H. pumilio, from people in Champasak province is novel. However, recovery of O. viverrini was previously reported in 3 people (5, 10, and 395 specimens) residing near Pakse, the capital of Champasak province [7]. No intestinal flukes were recovered from these 3 people [7]. Therefore, in the present study, it was surprising to see that the worm load of H. taichui and H. pumilio was markedly higher than that of O. viverrini in Champasak province. One patient, a 35-year-old man, expelled as many as 129,159 specimens of H. taichui, and thus he represents the most heavily infected case with H. taichui ever recorded in the literature. Details of other intestinal fluke infections and T. saginata will be published separately.
The hyperendemicity of H. taichui infection among riparian people in Saravane Province was closely correlated with the report of metacercarial prevalence in fish in Saravane Province [17]. H. taichui metacercariae were detected in various freshwater fish species from Saravane that included Hampala dispar, Cyclocheilichthys enoplos, Mystacoleucus greenwayi, and Puntioplites proctozysron with the average metacercarial density per fish of 1,532 (range 16-6,050), 346 (14-986), 337 (8-1,625), and 175 (2-863), respectively [17]. However, the metacercariae of O. viverrini were also detected heavily in H. dispar with the average number per fish of 453 [17]. No or very few O. viverrini metacercariae were detected in other species of fish examined in Saravane Province [17]. It is strongly suggested that H. dispar is an important source of infection both for H. taichui and O. viverrini in this area.
The present study indicated that the sole use of fecal examinations to detect helminth eggs does not fully allow the determination of the actual prevalence and intensity of liver and intestinal flukes in Lao PDR. For example, 2 recent studies performed in Champasak province reported the results of fecal examinations on the residents [18-20]; the STE were interpreted only as O. viverrini eggs, and the possibility for them to be eggs of intestinal flukes, in particular, Haplorchis spp., was overlooked. The adult worm recovery after chemotherapy and purgation, like our studies [10,11,14-16] and others [13], is helpful to determine the actual and relative predominance of liver and intestinal flukes in each area, although it is a tedious work and needs experts who have much experience and skill. It would be preferable to have a proper technique to distinguish the species of STE in fecal specimens.
Several diagnostic techniques have been reported to be useful for morphologic discrimination of STE in fecal samples [21-23]. Iodine staining was helpful for discriminating lecithodendriid eggs (P. molenkampi and P. bonnei) from those of O. viverrini [21]. Potassium permanganate temporary staining, using 1% (w/v) solution for 1 min, was also applied to discriminate the eggs of O. viverrini, H. taichui, and P. bonnei [23].
Molecular techniques have been applied to detect O. viverrini DNA in fecal samples [24-26]. In Khon Kaen, Thailand, a 98% specificity and a 100% sensitivity of the PCR technique were obtained in cases of moderate to severe infections (>1,000 EPG) but only a 68% sensitivity was shown in light infections (<200 EPG) [24]. In Lao PDR, the PCR sensitivity was lower; only around 50% in cases even with high EPG counts >1,000 [25]. The possible presence of PCR inhibitors in the feces was suggested [25]. Cetyltrimethyl-ammoniumbromide was used to remove such inhibitors, which resulted in an enhanced sensitivity of PCR technique to detect fecal O. viverrini DNA, from 44.8% to 79.3% [26]. It was stated that the primers used for PCR did not cross-react with Haplorchis spp. [25]. In this respect, the possibility of mixed infections with O. viverrini with minute intestinal flukes, including Haplorchis spp., was raised as a reason for low sensitivity of PCR technique to detect O. viverrini DNA [25,26]. Subsequently, PCR assays to discriminate O. viverrini from those of H. taichui and H. pumilio were developed using the internal transcribed spacer (ITS) regions, ITS1 and ITS2 [27]. The PCR amplicons of O. viverrini, H. taichui, and H. pumilio were 800, 930, and 1,250 bp, respectively, for ITS1, which successfully differentiated the 3 species, whereas those for ITS2 were 380, 530, and 380, respectively, which could not discriminate O. viverrini and H. pumilio [27]. The sensitivity of ITS1 PCR using fecal samples, however, was relatively low (76.2%). Further studies are needed before they can be used practically as a coprodiagnostic tool [27].
It may be argued that not all of the O. viverrini worms were expelled from the subjected cases by a 40 mg/kg single dose treatment with praziquantel. This possibility cannot be completely ruled out. However, in our previous studies in Vientiane municipality and Savannakhet province, the same protocol as in the present study was applied, and 3-315 O. viverrini specimens in Vientiane and 1-1,350 O. viverrini specimens in Savannakhet were recovered individually in the diarrheic stools of the subjects within 5-6 hr (4-5 successive stools) after praziquantel administration [10,11]. These observations indicate that if a person is infected with O. viverrini, a majority, if not all, of the worms are expelled by this procedure. A previous study in Thailand supports this hypothesis; in 9 patients treated with 40 mg/kg praziquantel in a single dose followed by purging and whose diarrheal feces were collected at least 24 hr after purgation, 95% of all worms were expelled within the first 4 hr [28]. A study performed in Khon Kaen, Thailand, a hyperendemic area of opisthorchiasis, reported that the worm load of O. viverrini among 181 human autopsy cases averaged 182.4 and ranged from 1-2,946 per individual [29]. In our previous studies in Savannakhet and Vientiane [10,11], the average worm load measured by worm recovery after praziquantel treatment and purging was 115.4 (n=29; 0-1,350 per individual) and 57.8 (n=18; 3-315 per individual), respectively. Therefore, it is suggested that the procedure we used is a reliable method for recovery of both liver and intestinal flukes from humans.
ACKNOWLEDGMENTSWe thank the staff of the Center for Laboratory and Epidemiology, Department of Hygiene and Prevention, Ministry of Public Health, Vientiane, and the staff of the Saravane and Champasak Provincial Health Department, Lao PDR, for their help in collection of fecal samples and preparation of Kato-Katz smears.
REFERENCES1. Chai JY, Shin EH, Lee SH, Rim HJ. Foodborne intestinal flukes in Southeast Asia. Korean J Parasitol 2009;47(suppl):S69-S102. PMID: 19885337.
2. Chai JY, Murrell KD, Lymbry A. Fishborne parasitic zoonoses: status and issues. Int J Parasitol 2005;35:1233-1254. PMID: 16143336.
3. Chai JY, Lee SH. Food-borne intestinal trematode infections in the Republic of Korea. Parasitol Int 2002;51:129-154. PMID: 12113752.
4. Sripa B, Kaewkes S, Intapan PM, Maleewong W, Brindley PJ. Food-bone trematodes in Southeast Asia: epidemiology, pathology, clinical manifestation and control. Adv Parasitol 2010;72:305-350. PMID: 20624536.
5. Sornmani S, Pathammavong O, Bunnag T, Impand P, Intarakhao C, Thirachantra S. An epidemiological survey of human intestinal parasites in Vientiane, Laos. Southeast Asian J Trop Med Public Health 1974;5:541-546. PMID: 4477408.
6. Kobayashi J, Vannachone B, Xeutvongsa A, Manivong K, Ogawa S, Sato Y, Pholsena K. Prevalence of intestinal parasitic infection among children in two villages in Lao PDR. Southeast Asian J Trop Med Public Health 1996;27:562-565. PMID: 9185270.
7. Chai JY, Hongvanthong B. A small-scale survey of intestinal helminthic infections among the residents near Pakse, Laos. Korean J Parasitol 1998;36:55-58. PMID: 9529864.
8. Rim HJ, Chai JY, Min DY, Cho SY, Eom KS, Hong SJ, Sohn WM, Yong TS, Deodato G, Standgaard H, Phommasack B, Yun CY, Hoang EH. Prevalence of intestinal parasite infections on a national scale among primary schoolchildren in Laos. Parasitol Res 2003;91:267-272. PMID: 14574555.
9. Giboda M, Ditrich O, Scholz T, Viengsay T, Bouaphanh S. Human Opisthorchis and Haplorchis infections in Laos. Trans R Soc Trop Med Hyg 1991;85:538-540. PMID: 1755066.
10. Chai JY, Park JH, Han ET, Guk SM, Shin EH, Lin A, Kim JL, Sohn WM, Yong TS, Eom KS, Min DY, Hwang EH, Phommasack B, Insisiengmay B, Rim HJ. Mixed infections with Opisthorchis viverrini and intestinal flukes in residents of Vientiane municipality and Saravane province in Laos. J Helminthol 2005;79:283-289. PMID: 16153322.
11. Chai JY, Han ET, Guk SM, Shin EH, Sohn WM, Yong TS, Eom KS, Lee KH, Jeong HG, Ryang YS, Hoang EH, Phommasack B, Insisiengmay B, Lee SH, Rim HJ. High prevalence of liver and intestinal fluke infections among residents of Savannakhet Province in Laos. Korean J Parasitol 2007;45:213-218. PMID: 17876167.
12. Sayasone S, Tesana S, Utzinger J, Hatz C, Akkavong K, Odermatt P. Rare human infection with the trematode Echinochasmus japonicus in Lao PDR. Parasitol Int 2009;58:106-109. PMID: 19059359.
13. Sayasone S, Vonghajack Y, Vanmany M, Rasphone O, Tesana S, Utzinger J, Akkhavong K, Odermatt P. Diversity of human intestinal intestinal helminthiasis in Lao PDR. Trans R Soc Trop Med Hyg 2009;103:247-254. PMID: 19038411.
14. Chai JY, Han ET, Shin EH, Sohn WM, Yong TS, Eom KS, Min DY, Um JY, Park MS, Hoang EH, Phommasack B, Insisiengmay B, Lee SH, Rim HJ. High prevalence of Haplorchis taichui, Prosthodendrium molenkampi, and other helminth infections among people in Khammouane Province, Lao PDR. Korean J Parasitol 2009;47:243-247. PMID: 19724697.
15. Chai JY, Yong TS, Yong TS, Eom KS, Min DY, Shin EH, Banouvong V, Insisiengmay B, Insisiengmay S, Phommasack B, Rim HJ. Prevalence of the intestinal flukes Haplorchis taichui and H. yokogawai in a mountainous area of Phongsaly Province, Lao PDR. Korean J Parasitol 2010;48:339-342. PMID: 21234239.
16. Chai JY, Sohn WM, Yong TS, Eom KS, Min DY, Hoang EH, Phommasack B, Insisiengmay B, Rim HJ. Echinostome flukes recovered from humans in Khammouane Province, Lao PDR. Korean J Parasitol 2012;50:269-272. PMID: 22949759.
17. Rim HJ, Sohn WM, Yong TS, Eom KS, Chai JY, Min DY, Lee SH, Hoang EH, Phommasack B, Insisiengmay S. Fishborne trematode metacercariae in Luang Prabang, Khammouane, and Saravane Province, Lao PDR. Korean J Parasitol 2013;51:107-114. PMID: 23467784.
18. Sayasone S, Odermatt P, Phoumindr N, Vongsaravane X, Semsonbath V, Phetsouvanh R, Choulamany X, Strobel M. Epidemiology of Opisthorchis viverrini in a rural district of southern Lao PDR. Trans R Soc Trop Med Hyg 2007;101:40-47. PMID: 16828134.
19. Sayasone S, Mak TK, Vanmany M, Rasphone O, Vounatsou P, Utzinger J, Akkhavong K, Odermatt P. Helminth and intestinal protozoa infections, multiparasitism and risk factors in Champasak province, Lao People's Democratic Republic. PLoS Negl Trop Dis 2011;5:e1037. PMID: 21532735.
20. Forrer A, Sayasone S, Vounatsou P, Vonghachack Y, Bouakhasith D, Vogt S, Glaser R, Utzinger J, Akkhavong K, Odermatt P. Spatial distribution of, and risk factors for, Opisthorchis viverrini infection in southern Lao PDR. PLoS Negl Trop Dis 2012;6:e1481. PMID: 22348157.
21. Kaewkes S, Elkins DB, Sithithaworn P, Haswell-Elkins MR. Comparative studies on the morphology of the eggs of Opisthorchis viverrini and lecithodendriid trematodes. Southeast Asian J Trop Med Public Health 1991;22:623-630. PMID: 1820653.
22. Sripa B, Bethony JM, Sithithaworn P, Kaewkes S, Mairiang E, Loukas A, Mulvenna J, Laha T, Hotez PJ, Brindley PJ. Opisthorchiasis and Opisthorchis-related cholangiocarcinoma. Acta Trop 2011;120(Suppl 1):S158-S168. PMID: 20655862.
23. Sukontason K, Piangjai S, Sukontason K, Chaithong U. Potassium permanganate staining for differentiating the surface morphology of Opisthorchis viverrini, Haplorchis taichui and Phaneropsolus bonnei eggs. Southeast Asian J Trop Med Public Health 1999;30:371-374. PMID: 10774711.
24. Wongratanacheewin S, Pumidonming W, Sermswan RW, Pipitgool V, Maleewong W. Detection of Opisthorchis viverrini in human stool specimens by PCR. J Clin Microbiol 2002;40:3879-3880. PMID: 12354909.
25. Stensvold CR, Saijuntha W, Sithithaworn P, Wongratanacheewin S, Strandgaard H, Ørnbjerg N, Johansen MV. Evaluation of PCR based coprodiagnosis of human opisthorchiasis. Acta Trop 2006;97:26-30. PMID: 16253202.
26. Duenngai K, Sithithaworn P, Rudrappa UK, Iddya K, Laha T, Stensvold CR, Strandgaard H, Johansen MV. Improvement of PCR for detection of Opisthorchis viverrini DNA in human stool samples. J Clin Microbiol 2008;46:366-368. PMID: 18003810.
27. Sato M, Thaenkham U, Dekumyoy P, Waikagul J. Discrimination of O. viverrini, C. sinensis, H. pumilio and H. taichui using nuclear DNA-based PCR targeting ribosomal DNA ITS regions. Acta Trop 2009;109:81-83. PMID: 18952037.
28. Ramsay RJ, Sithithaworn P, Prociv P, Moorhouse E, Mathaphat C. Density-dependent fecundity of Opisthorchis viverrini in humans, based on faecal recovery of flukes. Trans R Soc Trop Med Hyg 1989;83:241-242. PMID: 2609378.
29. Sithithaworn P, Tesana S, Pipitgool V, Kaewkes S, Pairojkul C, Sripa B, Paupairoj A, Thaiklar K. Relationship between faecal egg count and worm burden of Opisthorchis viverrini in human autopsy cases. Parasitology 1991;102:277-281. PMID: 1852493.
Fig. 1Map showing the surveyed areas of Lao PDR, Saravane province (A-F districts) and Champasak province (G-L districts). 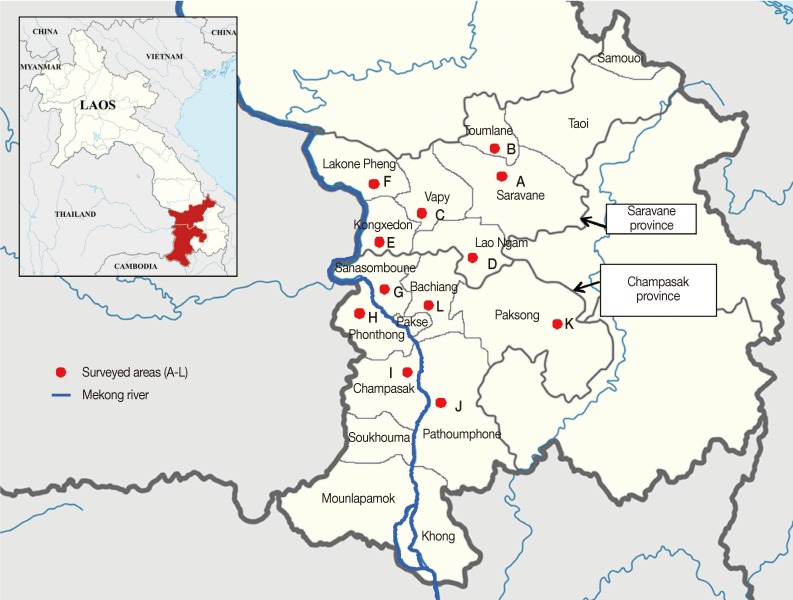
Table 1.Helminth eggs found in the feces of residents in Saravane and Champasak province, Laos from December 2009 to June 2010
Table 2.Adult flukes collected from residents in Champasak and Saravane Province, Laos after treatment with praziquantel from December 2009 to June 2010 |
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||