Intestinal helminthiases and schistosomiasis have long been recognized as human infections of significant public health importance especially in the tropics and are known to be usually more common in children than in adults (Nokes et al., 1991; WHO, 1993; Gillespie, 2001). Although relatively easy to control, several reports have shown that these human infections have remained endemic in many parts of the tropical world (Utzinger et al., 2002; Clennon et al., 2004; Poggensee et al., 2005).
Recent reports on intestinal helminthiases and schistosomiasis from Nigeria include those of Anosike et al. (2001), Bassey and Umar (2004), Ahmed et al. (2004), and Idowu and Rowland (2006). To the best of our knowledge, there is none on the epidemiology of intestinal helminthiasis from Ijebu-Ode Local Government Area (ILGA) and Odogbolu Local Government Area (OLGA) of Ogun State, southwest Nigeria. Moreover, the only previous report on urinary schistosomiasis involving school children in the 2 Local Government Areas was based exclusively on questionnaires (Ekpo and Mafiana, 2004).
The present study aimed to figure out the epidemiological picture of intestinal helminthiases and schistosomiasis among school children in some communities of OLGA and ILGA of Ogun State, southwest Nigeria. It is hoped that the findings of this study will assist the health planners and workers in the study area in their bid to provide health for all.
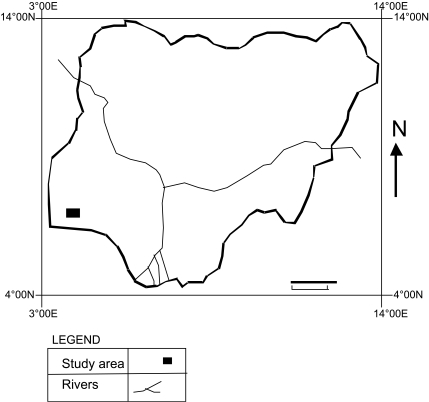
The study area consisted of Okun-Owa and Ijesha-Ijebu in OLGA, and Ijebu-Ode, Iloti, Odonoko, Irawo, Isiwo, and Odolewu in ILGA. Both Local Government Areas are in Ijebu division of Ogun State, Nigeria. The study area lies in the rainforest belt within latitudes 6° 30' and 6° 40' N, longitudes 3° 40' and 3° 50' E (Fig. 1). Okun-Owa and Ijesha-Ijebu are developing rural communities whose inhabitants are predominantly Yorubas (Ijebu dialect), who engage mainly in subsistence farming. Okun-Owa has 3 public schools, 1 public secondary school, while Ijesha-Ijebu has 1 public primary school. Each of the communities has 1 public primary health centre and a private clinic.
Ijebu-Ode is both urban and cosmopolitan, it is the headquarters of ILGA and its population consists of civil servants, artisans, traders and farmers. The town has 1 secondary health centre, many public and private health centers and about 30 public primary schools. Iloti, Odonoko, Irawo, Isiwo, and Odolewu are rural communities in ILGA. Each of the communities has a public primary school and a primary health centre. Many of the inhabitants are farmers.
In all the communities included in this study, potable water supply is infrequent, therefore, the inhabitants usually depend on streams (particularly in the rural communities), wells, bore-holes, harvested rain water (in rainy season) and mobile water tankers for their domestic water needs. Fecal disposal facilities used by the inhabitants of all the communities include water closet, pit latrines (commonest, especially in the rural areas) and open defecation.
Prior to the commencement of the study, permission was obtained from the local education authority of each of OLGA and ILGA. The head teacher and teachers of each selected school were contacted, and the parents and pupils were adequately enlightened on the purpose of the study. All the public schools in Okun-Owa, the public primary school in Ijesha-Ijebu, 8 randomly-selected public primary schools in Ijebu-Ode, and the public primary school in each of Iloti, Odonoko, Irawo, Isiwo, and Odolewu were included in the study. The examined population size was 1,059 (524 males, 535 females) and the age range was 3-18 years. A total of 662 and 397 subjects were examined in the rural communities and the urban center, respectively. The study was performed between June 2005 and November 2006.
For each participating school child, a questionnaire was administered to obtain information, such as age, sex, source of water for drinking, and other purposes, toilet facilities, and hygiene practices. Labeled sample bottles were distributed to the school children for a little portion of their early morning feces. In the laboratory, each collected sample was examined using direct fecal smear and brine concentration methods. For the brine concentration method, harvesting of helminth ova and larvae was done using coverslips, which was left on the brine-fecal sample suspension for 3-5 min. All microscopic observations were done with 10x objective and, when required, 40x objective lenses. Egg counts were recorded as no. of eggs/g of feces. The chi-square (χ2) test was used to compare data and to determine the significance of differences between prevalences.
Out of the 1,059 school children examined, 701 (66.2%) had one or more helminth infection (s). The helminths identified and their prevalences were Ascaris lumbricoides (53.4%; 565 cases), hookworms (17.8%; 189 cases), Trichuris tichiura (10.4%; 110 cases), Taenia sp (9.6%; 102 cases), Schistosoma mansoni (2.3%; 24 cases), Strongyloides stercoralis (0.7%; 7 cases), Schistosoma haematobium (0.6%; 6 cases), and Enterobius vermicularis (0.3%; 3 cases). The prevalence of A. lumbricoides was the highest, compared with other parasite species (P < 0.001). Table 1 compares the prevalences of the helminths among the urban center and the rural communities in the study area. The prevalence of T. trichiura in the rural communities was statistically higher than that in the urban community (P < 0.01). For A. lumbricoides, hookworms, Taenia sp, S. mansoni and S. stercoralis, the prevalences among the urban center and rural communities were similar (P > 0.05).
The gender-related prevalence of the helminths in the study area is shown in Table 2. Among males and females, A. lumbricoides revealed the highest prevalence (P < 0.001). Each of the recorded helminths had statistically similar prevalences among both genders (P > 0.05). The age-related prevalence of the helminths in the study area is summarized in Table 3. Ascaris lumbricoides showed the highest prevalence in all the age groups except 18+ years (P < 0.05). The 18+ years subjects had the statistically highest prevalence of T. trichiura (P < 0.001). For hookworms, 15-17 years age group had statistically highest prevalence (P < 0.05). The remaining helminths recorded had similar prevalences among the infected age groups (P > 0.05).
Ascaris lumbricoides had fertile and infertile eggs ratio of 13: 1 and 3.7: 1 in the urban centre and rural areas, respectively. In the study area, S. haematobium had overall mean intensity of 650 eggs/g. Among intestinal helminthes, A. lumbricoides had statistically highest mean intensity (565 eggs/g), followed by Taenia sp (475 eggs/g), hookworm (470 eggs/g), T. trichiura (460 eggs/g), S. stercoralis (190 larvae/g), E. vermicularis (150 eggs/g) and S. mansoni (145 eggs/g) (P > 0.05).
Among the infected school children, 244 (34.8%), 29 (4.2%), and 2 (0.3%) had double, triple and quadruple infections, respectively. The prevalences of double infections among males (48.4%) and females (51.6%) were statistically similar (P > 0.05). For double infections, Ascaris + hookworm combination had the statistically highest prevalence (45.9%), followed by Ascaris + Trichuris (26.2%), Ascaris + Taenia (16.0%), hookworm + Trichuris (3.7%), Ascaris + S. mansoni (2.9%), hookworm + Taenia (2.0%), hookworm + S. mansoni (1.2%), Ascaris + Strongyloides (0.8%), Trichuris + Taenia (0.8%), and S. mansoni + Taenia (0.4%) (P < 0.001). The prevalences of triple infection among males (37.9%) and females (62.1%) were significantly different (P < 0.02). The triple combination with the statistically highest prevalence was Ascaris + hookworm + Trichuris (48.3%), followed by Ascaris + hookworm + Taenia (17.2%), Ascaris + hookworm + S. mansoni (13.8%), Trichuris + Taenia + S. mansoni (10.3%), Ascaris + hookworm + Strongyloides (3.4%), Ascaris + Taenia + Trichuris (3.4%), and Ascaris + Taenia + S. mansoni (3.4%) (P < 0.001). The two cases of quadruple infection were found among females and the only combination recorded was Taenia + S. mansoni + E. vermicularis + S. stercoralis.
Observations from questionnaires showed that 13.5% of the school children examined practised open and indiscriminate defaecation, while 34.8% indulged in walking bare-footed. Among those positive for A. lumbricoides 65.8% drank well and/or stream water, 46.1% nibbled finger nails, 40.8% failed to wash hands and/or fruits before eating and 80.3% claimed having been dewormed ≤ one year earlier.
The high prevalence of parasitic helminths (66.2%) among school children in this study suggests a generally low standard of living and poor environmental sanitation in the study area (Ukoli, 1984; Smyth, 1996). The observation that A. lumbricoides had the highest prevalence in both the urban centre and rural communities agreed with the previous report of Ogbe et al. (2002) but disagreed with those of Nwaorgu et al. (1998) and Chhakda et al. (2006).The high prevalence of ascariasis among the children in the study area is corroborated by the relatively high occurrence of unhygienic habits among them. The similar prevalence of A. lumbricoides in the urban centre and rural communities possibly shows no difference among the communities in environmental sanitation and personal hygiene of the school children. The unhygienic practices among food vendors in the study area might have contributed to the occurrence of A. lumbricoides and some other helminthes among the school children (Idowu and Rowland, 2006). To the best of our knowledge, the report of the fertile and infertile eggs ratio of A. lumbricoides in this study is the first of its kind from Ogun State, southwest Nigeria. It is surprising that A. lumbricoides had higher proportion of fertile eggs in the urban centre than in the rural communities. This indicates the presence of relatively more viable transmissible A. lumbricoides eggs in the urban centre.
The prevalences of hookworm in the urban centre (17.9%) and the rural communities (17.8%) agreed with the report of Ogbe et al. (2002). However, the higher prevalence of T. trichiura in the rural communities compared to the urban centre is contrary to expectation in view of the fact that similar conditions generally enhance the endemicity of this infection, A. lumbricoides and hookworm (Ukoli, 1984; Piekarski, 1989). The reason for this discrepancy in the study area is not known. Taenia sp had similar prevalences in the urban centre and the rural communities. The presence of taeniasis in the study area might have been due partly to widespread habit of eating improperly-cooked beef (locally known as 'suya') and pork in the study area. Taeniasis had been reported previously from some other parts of Nigeria (Gundiri and Okwuosa, 2005) and elsewhere (Celiksoz et al., 2005). The prevalences of E. vermicularis and S. stercoralis were low in the study area. This might have been due to the diagnostic methods used in this study; particularly for E. vermicularis which is best diagnosed using cellophane tape smear methods (Shoup, 2001). The occurrence of S. mansoni in the study area conforms to some previous reports from Nigeria (Bassey and Umar 2004). The observation of S. haematobium eggs in feces of some school children in the study area agrees with the fact that they sometimes appear in the feces of infected persons (Smyth, 1996). The presence of schistosomiasis is no surprise since many of the school children had cause to frequent streams for drinking water, laundry, and other domestic purposes. Collection of edible freshwater snails (particularly Lanistes libycus) had been noted an important reason for water contact by many school children in many parts of southwestern Nigeria (Agbolade et al., 2004).
The study showed that although A. lumbricoides was most prevalent in both genders, none of the parasitic helminthes was gender-dependent in conformity with some previous reports (Mafiana and Omotayo, 1998; Taiwo and Agbolade, 2000). Generally, ascariasis decreased gradually in prevalence as the age of the school children increased. However, the high prevalence in virtually all age groups indicates general ignorance and/or deliberate neglect of basic rules of hygiene among the children. The observation of relatively higher prevalences of hookworm in age groups 12-14 and 15-17 years may be an indication of their higher level of involvement in farming activities than others. The relatively high prevalence of Taenia sp in children of 18 years age may be because they feel free in their communities and have more to spend on 'suya'. However, the reason for 18 years old children having highest prevalence of T. trichiura is not known. The absence of S. mansoni among 3-5 years age group may be because they make infrequent (if any) contact with natural water bodies. Normally, most of the eggs of S. haematobium are found in urine samples (Smyth, 1996). Therefore, a definite conclusion on the age-related occurrence of S. haematobium is difficult since no microscopic examination of urine samples was done in this study. Nevertheless, a study involving testing of urine samples with diagnostic reagent strips in the area will be reported in a later paper. The seeming restriction of S. stercoralis and E. vermicularis to certain age groups is attributable to their low prevalences in this study. The intensity of the helminthes appeared generally low in the study area.
In this study, the most common double infection was Ascaris + hookworm, while the most common triple infection was Ascaris + hookworm + Trichuris. These possibly indicate that the environmental conditions in the study area satisfied the development and successful transmission of A. lumbricoides, hookworm, and T. trichiura simultaneously (Ukoli, 1984).
This study has shown a general similarity in the epidemiological pictures of parasitic helminthes in the urban centre and the rural communities in the study area. This corroborates the opinion of Gillespie (2001) that urbanisation and population growth often combine to increase total burden of diseases in developing countries. It necessarily implies that there is an urgent need for concerted efforts towards ensuring adequate control of intestinal helminthiasis and schistosomiasis in OLGA and ILGA of Ogun State, Nigeria.