The protozoan parasite Toxoplasma gondii is an important cause of ocular diseases both in immunosuppressed and immunocompetent individuals (Tirard et al., 1991; Choi et al., 1997). Toxoplasma gondii can reach the eye through the bloodstream or be transmitted from the brain via the optic nerve (Roberts and McLeod, 1999). Active ocular toxoplasmosis consists of well-defined foci of coagulative necrosis of the retina or diffuse inflammation in the retina and the choroid. We described a toxoplasmic uveitis case focused on the difference in the retinal lesion and antibody titers after chemotherapy.
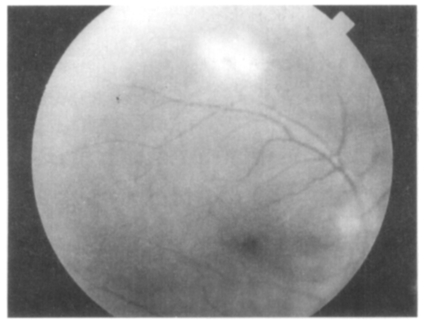
On December 15, 1997, a 60-year-old man visited out-patient clinic at the Department of Ophthalmology, Catholic University of Korea, College of Medicine, due to a decreased and blurred vision in his right eye which persisted for 2 weeks with slight muscle pain. He had no other previous problems with his general health, but he had been treated with oral antihypertensive drugs for 5 years. With a slit-lamp examination, mild inflammatory reaction was detected in the anterior chamber and vitreous body. Through an ophthalmoscopy, one optic disk-sized whitish retinal infiltration was observed in the superior temporal vascular area. One percent of prednisolone acetate (O-LON) solution was applied topically for 10 days (4 times/day). However, retinal infiltration continued to progress and sheath perivascularly on ophthalmoscopy, and hypofluorescent retinal area was detected on a fluorescein angiography. Retinal necrosis was suspected, thus 40 mg of prednisolone (H-LON) was orally administered 3 times a day. Two weeks later, the fundus examination of the right eye showed aggravated inflammation and retinal necrosis as shown in Fig. 1. Oral administration of prednisolone was terminated.
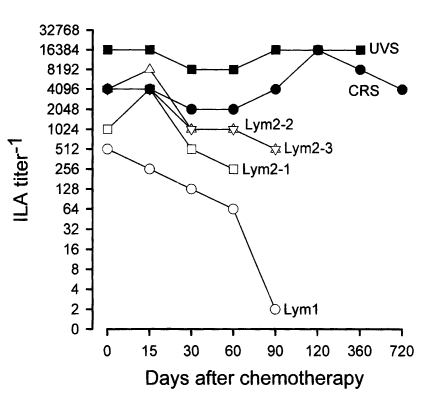
Serological tests for T. gondii were performed by IgG-ELISA and ILA, both of which resulted in strong positives, 1.02 for ELISA with a cut-off value of 0.25 and 1:16,384 for ILA with a cut-off value of 1:32. An oral combination therapy with Fansidar F (25 mg pyrimethamine plus 500 mg sulfonamide, Hoffmann-La Roche, Basel, Switzerland) and prednisolone was carried out for 8 weeks. Five weeks after chemotherapy, inflammatory cells could not be found in the anterior chamber, but there were still one or two positive reactions of inflammatory cells in the vitreous body. The whitish retinal necrotic lesion around the superior temporal vascular area disappeared and the pigmental change in the lesion was observed with the fundus examination. On July 8, 1998, the corrected visual acuity of the right eye improved to 0.63, and there was no inflammatory vitreous opacity. Only clear-cut margin of whitish retinal lesion was observed in the superior temporal vascular area of the right eye. However, antibody titers by ELISA and ILA were still in a high range until now (Fig. 2), dotted rectangle line (labeled by UVS). This is compatible with another chorioretinitis case (dotted circle, labeled by CRS, Choi et al., 1997) as described as limitations of relation between serological examination and the ocular pathology (Holliman et al., 1991), whereas those of lymphadenitis cases appeared to be decreased rapidly in antibody titers (Lym1 of Kim et al., 1993 and Lym2-1, 2-2, and 2-3 of Choi et al., 1997) after chemotherapy.
The patient has enjoyed eating rare-cooked steaks during his frequent visits to many European nations since his young age as an economic specialist. Most European nations are known to have high toxoplasmosis incidences epidemiologically where the meat harboring tissue cysts is the major source of infection (Dubey and Beattie, 1988). He may have been infected in the past without any recognized symptoms, but have become symptomatic by the reactivation of chronic infection presumed reduction in immunity (Holland et al., 1988) caused by extensive stress and excess fatigue to cope with the national economic crisis and IMF situation in Korea since the end of 1997.
Toxoplasmic retinochoroiditis is the major cause of visual impairment in the U.S.A. and the European nations, where it accounts for 30-50% of all cases of the posterior uveitis (McCannel et al., 1996). However, detection of retinal diseases caused by T. gondii are limited in Korea. There is a difference in toxoplasmic environment such as the low prevalence rate and titers of antibody (Choi et al., 1992) resulted from different food-eating habit and pet-loving fashion in Korea. Additionally, ocular toxoplasmosis has been paid less attention by clinicians in the fields of ophthalmologic and infectious diseases. However, as the living pattern changes gradually, the probability of T. gondii infection is expected to increase. We suggest that the patients of ocular inflammation should be checked serologically in order to diagnose toxoplasmosis or to rule out the possibility of infection prior to a corticosteroid treatment.