Subcapsular Splenic Hemorrhage in Vivax Malaria
Article information
Abstract
In malaria, splenic rupture is a serious complication potentially leading to death. Subcapsular hemorrhage of spleen is thought to be an impending sign of splenic rupture; however, the characteristics of subcapsular hemorrhage are not well known. We report 3 cases of subcapsular hemorrhage of the spleen in vivax malaria, with varying degrees of severity. Case 1 showed subcapsular hemorrhage without splenic rupture, was treated by antimalarial drug without any procedure. The healing process of the patient's spleen was monitored through 6 computed tomography follow-up examinations, over 118 days. Case 2 presented subcapsular hemorrhage with splenic rupture, treated only with an antimalarial drug. Case 3 showed subcapsular hemorrhage with splenic rupture and hypotension, treated using splenic artery embolization. They all recovered from subcapsular hemorrhage without any other complications. These 3 cases reveal the process of subcapsular hemorrhage leading to rupture and a potentially fatal outcome. The treatment plan of subcapsular hemorrhage should be determined carefully considering the vital signs, changes in hemoglobin, and bleeding tendency.
INTRODUCTION
Malaria is a protozoal disease that causes hundreds of thousands of annual deaths globally [1]. In Korea, Plasmodium vivax is the only prevalent species [2]. Vivax malaria was previously known as a benign disease, but cases of severe vivax malaria have been increasingly reported [3,4]. Among the various complications of vivax malaria, splenic rupture is an important complication that can lead to death [5]. Therefore, early diagnosis of splenic rupture is important; however, preceding signs or changes in the spleen are not well known in malaria cases. From January 2007 to July 2018, we treated 255 patients with vivax malaria and 3 of them had subcapsular hemorrhage in the spleen. We report 1 case of vivax malaria with subcapsular hemorrhage occurring immediately before spleen rupture and 2 cases of vivax malaria with subcapsular hemorrhage with splenic rupture.
CASE DESCRIPTION
Case 1
A 39-year-old man visited our hospital (Inha University Hospital, Incheon, Korea) with a febrile sensation since 1 week prior. On physical examination, his blood pressure was 120/80 mmHg, pulse rate was 80/min, respiratory rate was 20/min, and body temperature was 39°C. He had severe left upper abdominal pain and splenomegaly. On laboratory examination, he presented decreased hemoglobin (12.3 g/dl) and platelet count (22,000/μl). His prothrombin time (PT) was 1.00 (international normalized ratio, INR), activated partial prothrombin time (aPTT) was 41.0 seconds, total bilirubin was 2.5 mg/dl, and P. vivax parasitemia was 42,174/μl (Table 1). He was diagnosed with vivax malaria using rapid antigen testing (SD-Bioline Malaria-Ag-Pf/Pan™) and peripheral blood smear. Abdominal computed tomography (CT) was done for the evaluation of painful splenomegaly and showed subcapsular hemorrhage without splenic rupture. His hemoglobin decreased from 12.3 to 9.6 after 2 days, but vital signs were stable. He was observed without surgery or intervention. The patient was treated with chloroquine and primaquine, and he gradually improved and was discharged. Follow-up abdominal CT was performed on the 7th, 15th, 25th, 57th, and 118th day after first diagnosis (Fig. 1A).
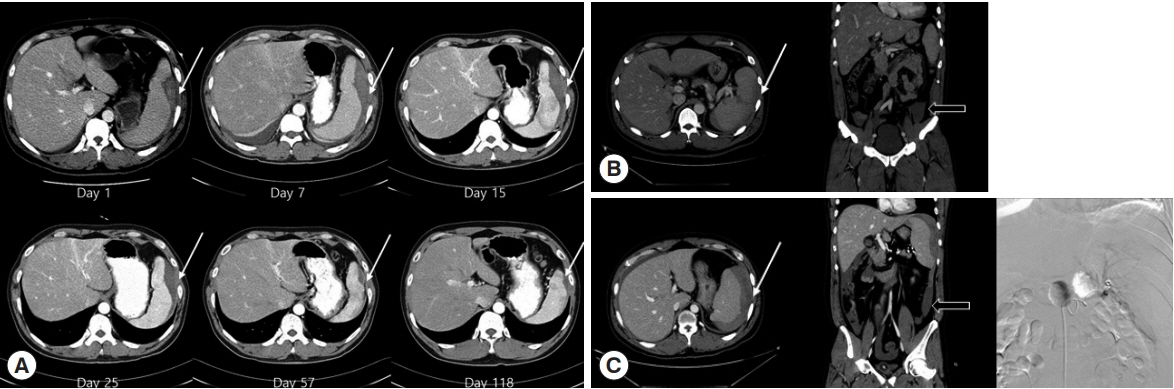
(A) Changes in splenic hemorrhage over time in Case 1: Subcapular hemorrhage of the spleen was found, without rupture. The subcapsular hemorrhage was absorbed slowly, over 118 days. (B) CT finding in Case 2: Subcapular hemorrhage with hemoperitoneum. (C) CT finding and coil embolization for splenic rupture in Case 3. White arrows: subcapsular hemorrhage. Black arrows: hemoperitoneum.
In summary, the above case showed subcapsular hemorrhage without splenic rupture. The patient experienced relatively rapid improvement with anti-malarial drugs, indicating the possibility that spleen capsule tension can be improved rapidly. Therefore, medical treatment and close observation can be considered a treatment option in the subcapsular hemorrhage stage. In addition, this case illustrated interesting changes and improvement in subcapsular hemorrhage with time, as seen in 6 CTs performed over 4 months.
Case 2
A 40-year-old man was admitted to a hospital in Incheon with fever and abdominal pain for the prior 5 days. He presented stable blood pressure and heart rate. His initial hemoglobin was 14.2 g/dl, platelet count was 35,000/μl, PT was 1.02 (INR), aPTT was 34.6 sec, and total bilirubin was 2.5 mg/dl. He showed a positive result in the malaria rapid antigen test (SD-Bioline Malaria-Ag-Pf/Pan™), and P. vivax was seen in a peripheral blood smear. He was immediately treated with chloroquine. However, the next day he experienced more severe abdominal pain and was transferred to our hospital. At the time of the visit to our hospital, his blood pressure was 133/63 mmHg, pulse rate was 96/min, respiratory rate was 18/min, and body temperature was 39.6°C. He was clearly conscious and there was no tendency of bleeding found in the mouth, anus, or urine. His hemoglobin was 13.4 g/dl (Table 1). He underwent CT for evaluation of the severe right upper abdominal pain, and splenic rupture was found with multifocal splenic infarction and subcapsular hemorrhage (Fig. 1B). The patient's vital signs were stable, and the patient did not want to undergo any surgery or intervention. After 2 days, the patient's hemoglobin dropped to 10.8. However, his vital signs were stable with no hypotension. On the 4th day, he was transferred out to another hospital uneventfully, and he is alive with no further problems 3 years later.
In summary, case 2 was an advanced case compared to case 1, and showed splenic rupture; however, the patient's condition was stable, and he recovered without surgery or intervention.
Case 3
A 38-year-old man visited our hospital [6]. He had undergone chemotherapy for extranodal marginal zone B-cell lymphoma of mucosa-associated lymphoid tissue and had no subsequent evidence of disease. When he visited our hospital, his blood pressure was 120, pulse rate was 80/min, respiratory rate was 20/min, and body temperature was 39°C. He presented a platelet count of 71,000/μl, serum bilirubin of 1.9 mg/dl, PT of 1.22 (INR), aPTT of 35.4 sec, and 14,019/μl of parasitemia (Table 1). Through rapid antigen testing (SD-Bioline Malaria-Ag-Pf/Pan™) and peripheral blood smears, he was diagnosed with vivax malaria. CT was performed for severe upper abdominal pain, and subcapsular hemorrhage of spleen and hemoperitoneum were seen on CT (Fig. 1C). The patient’s hemoglobin level was 14.4 g/dl on the first day and dropped to 9.5 the next day. He had continuous hypotension, and spleen angiography was conducted. There was no apparent extravasation of the contrast agent and embolization was performed. The patient was stable and there was no additional bleeding on CT 6 days later. After 8 days, CT showed no progression of hemorrhage. Subsequently, he was discharged without any further problems.
In summary, case 3 showed unstable vital signs and was more advanced than case 2. In splenic rupture with unstable vital signs, surgery or radiologic intervention should be considered. Recently, the use of embolization has been increasing after its development as an intervention. Case 3 is an example showing that intervention is an important treatment option in malarial splenic rupture.
DISCUSSION
In vivax malaria, the frequency of splenic rupture is unclear but is known to be less than 2% from previous studies [7]. Our study showed a similar incidence, but the incidence can be influenced by several variables including species, partial immunity due to frequent exposure, and accessibility to radiologic examination. Although the pathophysiology of splenic rupture is not well known, splenomegaly and increased tension of the splenic capsule are considered as the main causes of rupture. Considering the fact that there are several reports of splenic rupture in patients experiencing their first infection [8], the immune response appears to be strongly related to the rupture; however, no studies have addressed this hypothesis.
The 3 cases of this report may present a progress from subcapsular hemorrhage to stable rupture and unstable rupture. We hypothesize that subcapsular hemorrhage occurs first followed by rupture due to increased tension of the capsule resulting from the increasing hemorrhage. This progression is currently more likely to be observed because of increased accessibility to imaging studies. Moreover, the results of short-term follow-up imaging in case 1 using CT were interesting. In the serial CT images, splenic hemorrhage showed the process of healing, suggesting that spleen may be vulnerable to trauma for several months after the event.
All 3 patients had severe abdominal pain and a relatively rapid change in hemoglobin. It is important to confirm left upper abdominal pain in malaria patients. If suspicious, rapid imaging testing is necessary. Close monitoring is indispensable, especially for subcapsular hemorrhage. Medical treatments [9], embolization [6], and splenectomy [10] are considered for the treatment of splenic rupture. The treatment should be determined carefully considering the vital signs and bleeding tendency.
Severe vivax malaria complications were noted in Koreans with low partial immunity to malaria. Korea has a national health insurance system; thus, Koreans have high medical accessibility and the time from fever to the diagnosis of malaria is relatively short. Nonetheless, the incidence of high splenic hemorrhage (3/255) is likely associated with the low partial immunity of Koreans [3]. People from countries with low exposure to malaria, as well as those from Korea should pay close attention to the occurrence of serious complications associated with malaria infection.
In conclusion, we describe a case series of subcapsular hemorrhage with varying degrees of severity. Subcapsular hemorrhage can be considered an impending sign of spleen rupture. When malaria patients have severe upper abdominal pain, it is important to consider early radiologic examination.
ACKNOWLEDGMENT
This work was supported by a research grant from Inha University Hospital.
Notes
CONFLICT OF INTEREST
The authors declare that they have no competing interests.
