Three clinical cases of cutaneous larva migrans
Article information
Abstract
Three cases of cutaneous larva migrans (CLM) were diagnosed in a returnee from a trip to Thailand and in 2 domestic farmers during July and September, 2003. The linear and serpiginous skin lesions on the lower extremities were presented in all 3 cases. Routine laboratory findings were normal. In the imported case, a 650 × 30 µm sized filariform nematode larva, presumably a species of hookworm, was detected in the lesion. All cases were treated with 400 mg albendazole once daily for 3-5 days, and their skin lesions gradually improved. In the present study, a causative agent of CLM was isolated for the first time in the Republic of Korea. Moreover, we speculate that CLM is prevalent in farmers who are in frequent contact with soil in the Republic of Korea.
INTRODUCTION
CLM is a peculiar dermatitis caused by the infectious larvae of nematodes. It is more commonly caused by dog and cat hookworms, i.e., Ancylostoma caninum and A. braziliense, though other nematode larvae, such as, Uncinaria stenocephala, Bunostomum phlebotomum, Strongyloides spp. and Gnathostoma spp., act as rare causative agents (Davies et al., 1993; Lucchina and Wilson, 1999; Alonso, 2000). The typical clinical picture of CLM is characterized by an erythematous, linear or serpiginous, dermatitis tract (Elder et al., 1997, Alonso, 2000).
Recently CLM cases have increased in the Republic of Korea in parallel with the popularity of travel to tropical and subtropical regions (Jang et al., 1995; Lim et al., 1996; Lee et al., 1998; Chang et al., 1999; Kim et al., 1999; Park et al., 2001; You et al., 2002; Kwon et al., 2003; Suh et al., 2003). We report herein 3 cases of CLM, including 1 imported case, in which the causative larva, presumably a species of hookworm, was detected in the lesion, and 2 domestic cases. For morphological comparison, the third stage larvae of A. caninum were cultured from dog feces in an incubator at 30℃ using the filter paper culture method. Filariform larvae were collected from culture media at 15 days after incubation, and then observed and measured under a light microscope.
CASE RECORDS
Case 1
On July 2003, a 36-year-old house wife visited a local dermatology clinic in Jinju-si, Gyeongsangnamdo (Province), with linear and serpiginous skin lesions on both feet (Fig. 1). She had returned from a trip to Thailand some 10 days previously, and her skin symptoms appeared 8 days before her visit to our clinic. The routine laboratory findings were in the normal range, and a pathological examination of biopsied skin showed infiltrations of moderate perivascular lymphocytes and eosinophils in the upper dermis (Fig. 2). Moreover, a nematode larva was detected in a scratched lesion specimen (Fig. 3-A). The larva was 650 × 30 µm in size with a filariform esophagus of 175 µm. Its body to esophagus length ratio was 3.7 : 1, and its body length to width ratio was 21.7 : 1. The patient was treated with 400 mg/day of albendazole for 5 days. Her skin lesions were clearly improved 2 months after this treatment (Fig. 4).
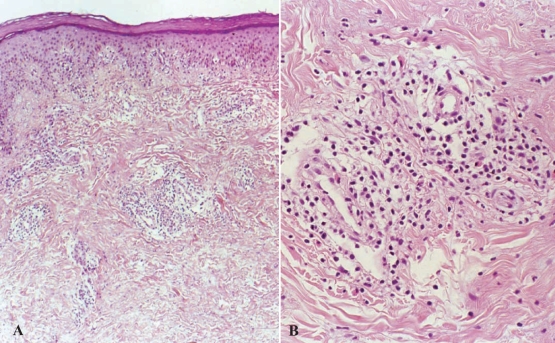
A: Histopathological findings of Case 1, which showed moderate lymphocyte and eosinophil infiltration. B: Magnified view of a part of Fig. 2-A.

A: Larva detected from a skin lesion of Case 1 with a long esophagus (E) and a pointed tail. B: A. caninun larva obtained by the fecal culture method shared these morphologic features.

Skin lesions on both feet of Case 1 had almost disappeared at 2 weeks after treatment with albendazole 40 mg once daily for 5 days.
For the identification of the isolated larva, we cultured A. caninum larvae in vitro and compared both larvae under the light microscope. Filariform larvae of A. caninum collected from egg-culture medium were 576-625 (average 605) × 23-25 (average 24) µm in size, and had a filariform esophagus of 145-153 (average 150) µm in length (Fig. 3-B). The ratios of body length to esophagus length and of body length to body width were 4.0 : 1 and 25.2 : 1, respectively.
Case 2
A 74-year-old man, a farmer residing in the small village of Kosung-gun, Gyeongsangnam-do, visited a local dermatology clinic on September 2003 with linear and serpiginous skin lesions on his right ankle and calf (Fig. 5). He had worked in a rice paddy 2 days previously, and had no experience of foreign travel. All laboratory findings including eosinophil count were in the normal range. He also said that many residents in his village presented same skin symptoms. The patient was treated with 400 mg/day of albendazole for 3 days, and his skin lesions were improved about 25 days after this treatment.
Case 3
A 62-year-old man, a farmer residing in Jinju-si, Gyeongsangnam-do, visited a local dermatology clinic with linear and serpiginous skin lesions on his left foot on September 2003 (Fig. 6-A). He also had no experience of foreign travel. Laboratory findings were in the normal range, and he too reported that some of his neighbors have similar skin lesions. He was treated with 400 mg of albendazole once daily for 3 days, and his skin lesions resolved without a relapse 4 months later (Fig. 6-B).
DISCUSSION
In the present study, a causative agent of CLM was isolated in the skin lesion of a patient for the first time in the Republic of Korea, although a sectioned larva was previously reported in a histopathologic specimen of a skin lesion (Chang et al., 1999; Park et al., 2001). It is known that the causative larvae of CLM are usually found in tunnels at the dermo-epidermal junction. However, as the larva in the present case was detected in a scratch, its precise location could not be determined.
We regret that the definitive identification of the nematode species involved was impossible, because only 1 worm was detected and the filariform larvae of different hookworm species are very similar in size and morphology. We compared A. caninum larvae experimentally cultured from dog feces with the larva obtained from the patient, and the A. caninum larvae were found to be slightly smaller than the larva obtained from the present case. Other morphologies were very similar, but no conclusion could be drawn concerning its identification. Systematic studies are required for the identification of the filariform larvae of hookworms.
The larvae of A. braziliense that penetrate the skin may survive for weeks or even months, and migrate through subcutaneous tissues, whereas A. caninum larvae encyst and remain dormant in the skin after a shorter cutaneous migratory period (Markell et al., 1999). Clinically, the CLM lesions induced by A. braziliense are pruritic and continuously linear in shape, whereas those by A. caninum are less pruritic with temporary urticarial symptoms, and intermittently linear in shape. Moreover, CLM lesions caused by U. stenocephala (the European dog hookworm) and B. phlebotomum (the cattle hookworm) are milder than those by A. braziliense with shorter migratory periods (Elder et al., 1997). The CLM lesions in all 3 of the described cases showed findings similar to those of A. braziliense.
CLM occurs world-wide, but is substantially more common in the tropics and subtropics. Occasional cases have been reported in non-endemic temperate regions (Blackwell and Vega-Lopez, 2001). In the Republic of Korea, a total of 13 such cases have been reported to date, 11 of these involved infections contracted overseas and only 2 had an indigenous origin (Jang et al., 1995; Lim et al., 1996; Lee et al., 1998; Chang et al., 1999; Kim et al., 1999; Park et al., 2001; You et al., 2002; Kwon et al., 2003; Suh et al., 2003). The present study adds 3 CLM cases, 1 imported from Thailand and 2 indigenous cases to Korean records. In particular, 10 of 12 imported cases had traveled in Southeast Asia, i.e., in Thailand, the Philippines, Indonesia, Vietnam and Cambodia. In the Republic of Korea, CLM is viewed as an important imported disease rather than as an indigenous disease, and therefore, we alert physicians to the possibility of creeping skin eruptions in those who have recently traveled to tropics or subtropics.
Albendazole is a powerful antihelminthic against infections by intestinal nematodes, and was first used to treat CLM in 1982. Many subsequent reports testify to its efficacy (Coulaud et al., 1982; Williams and Monk, 1989; Jones et al., 1990; Sanguigni et al., 1990; Rizzitelli et al., 1997; Veraldi and Rizzitelli, 1999; Kim et al., 2002; You et al., 2002; Suh et al., 2003). Thus, we also adopted an albendazole approach to treat the described 3 cases at a dose of 400 mg once daily for 3-5 days. All cases had a satisfactory result, skin lesions resolved without relapse at follow-up examinations.
More recently, ivermectin has been used to treat CLM. When a single dose of 12 mg of ivermectin was used in an open randomized study of 21 patients, it was found to be more effective than a single dose of 400 mg of albendazole (Caumes et al., 1993). In a review by Blackwell and Vega-Lopez (2001), all of the 10 CLM patients treated with ivermectin were completely cured without relapse. Thiabendazole is also known to be effective at treating CLM. However, ivermectin and thiabendazole are not freely available in hospitals. Therefore, we recommend albendazole at 400 mg once daily for 3 days as an effective regimen for the treatment of CLM.


